One of the aspects of gait analysis that I didn’t cover in any particular depth in my book was how to select data from a number of trials that is in someway representative of the patient. I think one of the reasons for this is because I couldn’t easily get my hands on any data that illustrated the issues well. In some ways this speaks for itself – in my experience large inter-trial variability, larger enough to affect how we interpret data, is actually quite rare in clinical practice. If the variability is small then it doesn’t really matter what technique you choose.
My personal preference is to avoid the issue altogether by overplotting data from multiple trials on the same graphs (similar to the graphs on the left above but with data from the other side plotted in a different colour as well). In this way you can take into account both the general pattern and the variability when interpreting the data. Some people object that using this technique it can be difficult to appreciate subtle features in individual traces, but there is a real question as to whether you should be even looking at such features if they are not consistent from trace to trace.
Now I’ve started annotating graphs with symbols to identify specific features in the data, however, I find that the combination of symbols and multiple curves can be a bit too messy and have resorted to looking to a single trace that can be taken of as representative. Although alternatives have been proposed I use the average trace. It leads to a little smoothing of the data – which isn’t perfect – but none of the other techniques are perfect either. It was interesting last week to come across a patient’s data that illustrated beautifully the problems of doing this.
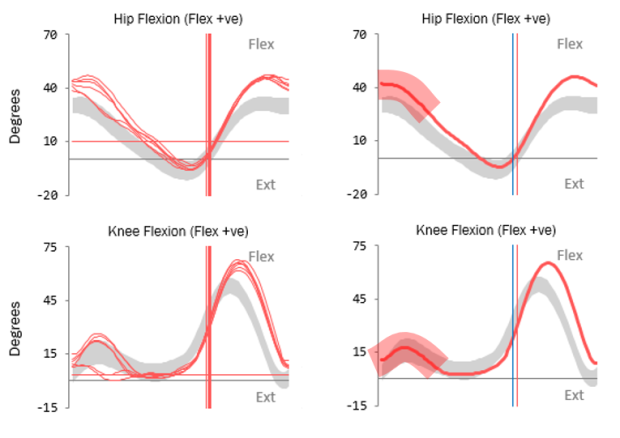
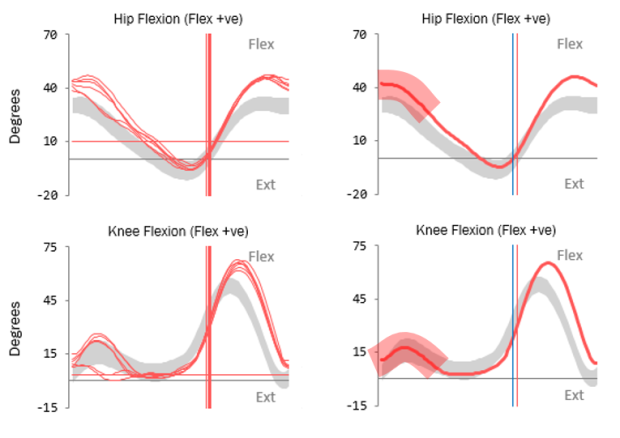
You can see the knee and hip traces here with the individual traces overlaid on the left and the averaged data plotted on the right. The problem is with the left knee. You can see that the patient exhibits two distinct patterns of knee movement in early stance (but remarkable repeatability elsewhere in the gait cycle). She either walks with full knee extension in early stance or with quite marked knee flexion. In the fully extended pattern her knee is more posterior and so there is increased hip extension as well (there is an effect on ankle dorsiflexion as well which I haven’t plotted). The average trace for the knee, however, falls well within normal limits and if you only ever looked at that trace you would never know that there was anything wrong with the knee.
None of the methods that are commonly used to generate a representative trace whether they be through picking one particular trace or providing some sort of averaging (mean or median) will result in something that represents the patient. The fundamental reason these don’t work is that this person’s gait is not characterised by one gait pattern, but by two, which she alternates between. It is not possible to understand her walking on a single curve, you need to look at multiple trials.
So although such issues don’t arise very often we don’t have a good way dealing with them in how we plot out or mark-up our data. What is needed is not a way of selecting single trace but a means of indicating that any single trace is unrepresentative. The broad semi-transparent bands on the right hand graphs are supposed to indicate that the trace cannot be appropriately interpreted without referring to the multiple trial data. I’ve now added them to the list of symbols that we use for marking up our graphs.
(PS The idea for a symbol to indicate underlying variability in the multiple trial data was first suggested to me by Sheila Gibbs in Dundee during an early consultation on the Impairment Focussed Interpretation methodology I outline in my book.)
(PPS if you do feel a need to select a representative trace and want to do this systematically then a robust method is presented by Morgan Sangeux in this recent paper. It is however worth noting that in the example he gives in Figure 1 the trace chosen as most representative overall does not give a good indication of the underlying data for either pelvic tilt or foot rotation despite the rigour of the technique.)